45 YEAR OLD FEMALE WITH ? ACUTE GASTROENTERITIS
GM CASES
Date of admission: 7/8/2021.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This is a case of 45 year old female, farmer by occupation,resident of gummarvai,chityala, came to the casualty on 7/8/21 with c/o vomiting and loose stools since 15 days.
The patient was apparently asymptomatic 6 months back, where she had h/o fever, she consulted near by RMP doctor, she was on injections for 2 days. Then she got back into health for next 2 months , doing her daily work of agriculture and household activities.
After 2 months she had history of loss of appetite and history of weight loss significantly upto ~10 kg, and the fever reverted back, then they took her to a hospital, near nalgonda, where all her necessary investigations were done and the patient was prescribed necessary medication and sent back home.
She started deteriorating and was on EMPIRICAL ATT , which she used for 15 days and stopped later.
Then from 11/7/21 she developed vomiting, loose stools and abdominal pain, for which she was taken to ANOTHER HOSPITAL,on 26/7/21. Where she was treated conservatively for above symptoms and the reports say that she also had mouth ulcers and generalised weakness. Episodes of Vomiting and loose stools were relieved,other symptoms persisted , patient now had a burning sensation in throat, for which she was again treated conservatively in the same hospital on 31/7/21.
Symptoms were on and off since 11/7/21.
Now the patient again came to our hospital with the similar complaints of loose stools and vomiting.
LOOSE STOOLS- > 6 episodes ,large in volume, watery consistency, not a/w any mucus/blood, no pain abdomen.
VOMITING-> 6 episodes, non projectile, contains food particles,non foul smelling.
for which she was admitted and was diagnosed as ? ACUTE GASTROENTERITIS.
The patient was subjected to various tests as a part of routine investigations, where she was detected RETRO POSITIVE DENOVO.
Past illness-
No history of of DM/HTN/asthma /epilepsy/ TB.
There is history of blood transfusion 16 years back due to hysterectomy where she had significant blood loss.
Treatment history -ATT for 15 days and discontinued.
Personal history-
-diet mixed .
-decreased appetite .
-bowel and bladder movements: H/o loose stools since 15 days.
-no addictions.
- sleep: adequate.
Family history-not significant
General Examination-
Patient is conscious, coherent and cooperative.
Pallor present
no icterus, no clubbing, no cyanosis, no lymphadenopathy,no edema.
Vitals-
PR-84 bpm.
BP-130/ 80 mm Hg.
RR-16 cpm.
GRBS- 110 mg/dl.
Temperature-afebrile.
SpO2-98%
Systemic examination-
CVS- S1, S2 heard, no murmurs, no added sounds.
RS- BAE+,NVBS heard, trachea central in position.
P/A- soft, non-tender, no palpable mass or swelling.
CNS- NAD.
Provisional Diagnosis-
? ACUTE GASTROENTERITIS.
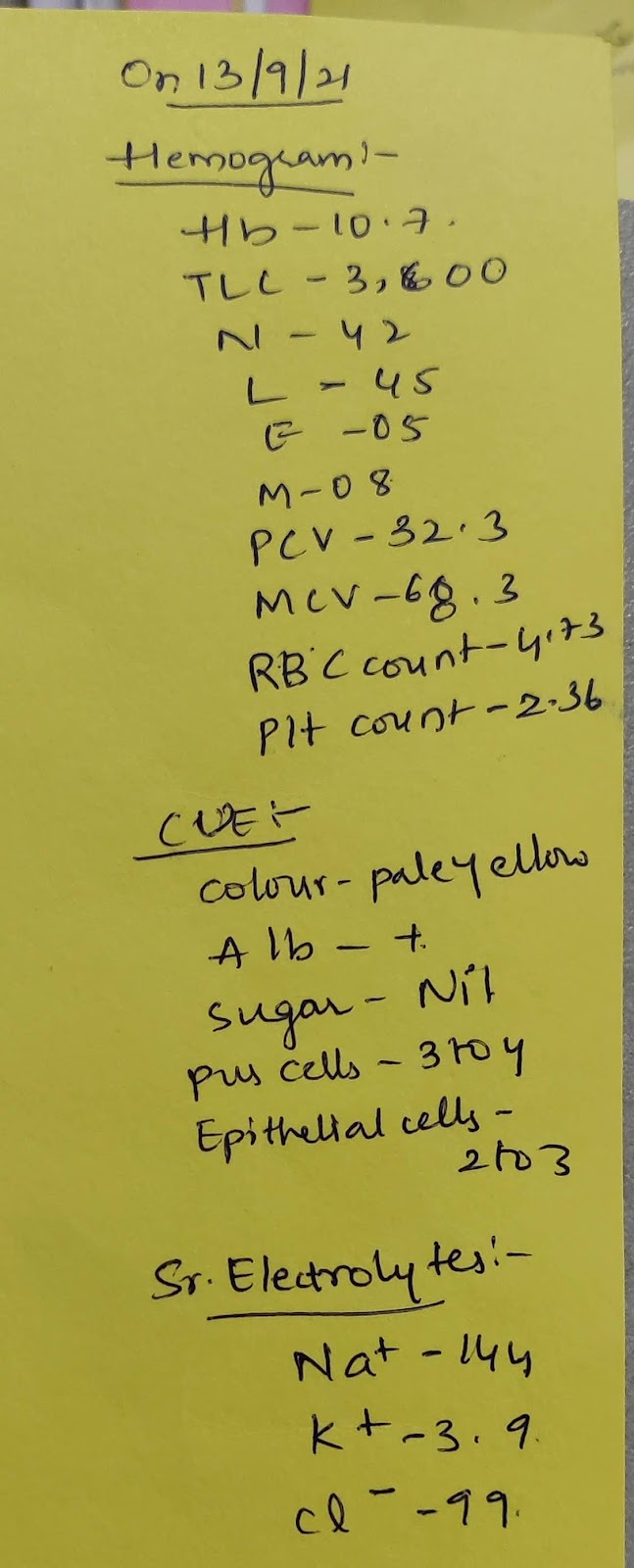
Investigations
ON 9/8/21:
ON 10/8/21
CLINICAL IMAGES
SOAP NOTES- 45 YR OLD FEMALE
DIAGNOSIS- ? ACUTE GASTROENTERITIS.
DAY 1 (7/8/21)SOAP
SUBJECTIVE
loose stools 6 episodes.
vomitings 6 episodes .
OBJECTIVE
TEMP-98.5 F
PR- 84bpm
BP-130/80mm hg
RR-16 cpm.
ASSESSMENT
? ACUTE GASTROENTERITIS,
PLAN OF CARE:
IVF- NS,RL @75ML/HR .
INJ METROGYL 500ML IV TID
INJ CIPROFLOXACIN 500 MG IV BD
ORS-1 PACKET IN 1 L WATER, 200 ML AFTER EVERY EPISODE OF STOOLS.
INJ PAN 40 MG IV OD
INJ ZOFER 4MG IV TID
BP/PR/SPO2/TEMP CHARTING 4TH HOURLY.
DAY 2 SOAP
SUBJECTIVE
loose stools 4 episodes.
vomitings.
OBJECTIVE
TEMP-98 F
PR-84 bpm
BP-100/60 mmhg
RR-18cpm.
ASSESSMENT
?ACUTE GASTROENTERITIS
RVD+(NEWLY DETECTED)
RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE
IVF- NS,RL @75ML/HR .
INJ METROGYL 500ML IV TID
INJ CIPROFLOXACIN 500 MG IV BD
INJ PAN 40MG IV OD
INJ ZOFER 4MG IV TID
BP,PR,RR,TEMP MONITORING 6TH HRLY
TAB FLUCONAZOLE 150 MG PO OD.
DAY 3 SOAP
SUBJECTIVE
loose stools 3 episodes.
OBJECTIVE
TEMP - 101 F
PR-100 bpm
BP-100/70 mmhg
RR- 18 cpm
ASSESSMENT
? ACUTE GASTROENTERITIS
RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE
IVF NS,RL@75ML/HR.
INJ METROGYL 500ML.IV TID.
INJ CIPROFLOXACIN 500MG IV BD.
INJ FLUCONAZOLE 150MG PO OD.
INJ PAN 40MG IV OD.
INJ ZOFER 4MG IV TID.
SOAP NOTES DAY 4
SUBJECTIVE
LOOSE STOOLS 1 EPISODE.
OBJECTIVE- TEMP: 97.3F
PR- 90 BPM
BP- 100/70 MMHG
RR- 18CPM.
ASSESSMENT: ? ACUTE GASTROENTERITIS, RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE:
IVF NS,RL@75ML/HR.
INJ METROGYL 500ML.IV TID.
INJ CIPROFLOXACIN 500MG IV BD.
INJ FLUCONAZOLE 150MG PO OD.
INJ PAN 40MG IV OD.
INJ ZOFER 4MG IV TID.
Tab SEPTRAN DS(800MG/160MG) PO OD.
SOAP NOTES DAY 5
SUBJECTIVE
NO NEW COMPLAINTS
O- TEMP: 99F
PR- 88 BPM
BP- 90/70 MMHG
RR- 19CPM.
ASSESSMENT: ? ACUTE GASTROENTERITIS, RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE:
IVF NS,RL@75ML/HR.
INJ METROGYL 500ML.IV TID.
INJ CIPROFLOXACIN 500MG IV BD.
TAB FLUCONAZOLE 150MG PO OD.
INJ PAN 40MG IV OD.
INJ ZOFER 4MG IV TID.
Tab SEPTRAN DS(800MG/160MG) PO OD.
SOAP NOTES DAY 6
A 45 YR OLD FEMALE WITH ACUTE GASTROENTERITIS
RETRO POSITIVE (NEWLY DETECTED)
PRE RENAL AKI (RESOLVED)
SUBJECTIVE
NO NEW COMPLAINTS
O- TEMP: 99F
PR- 82BPM
BP- 100/80 MMHG
RR- 19CPM.
ASSESSMENT: ACUTE GASTROENTERITIS, RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE:
IVF NS,RL@75ML/HR.
INJ METROGYL 500ML.IV TID.
INJ CIPROFLOXACIN 500MG IV BD.
TAB FLUCONAZOLE 150MG PO OD.
INJ PAN 40MG IV OD.
INJ ZOFER 4MG IV TID.
Tab SEPTRAN DS(800MG/160MG) PO OD.
SOAP NOTES DAY 7
A 45 YR OLD FEMALE WITH ACUTE GASTROENTERITIS
RETRO POSITIVE ( NEWLY DETECTED)
PRE RENAL AKI secondary to GE ( RESOLVED)
SUBJECTIVE
NO NEW COMPLAINTS
O- TEMP: 96.6F
PR- 62BPM
BP- 90/70 MMHG
RR- 17CPM.
ASSESSMENT: ACUTE GASTROENTERITIS, RETRO POSITIVE WITH ORAL CANDIDIASIS.
PLAN OF CARE:
TAB FLUCONAZOLE 150MG PO OD.
INJ PAN 40MG IV OD.
INJ ZOFER 4MG IV TID.
COLLECT CD4 COUNT.
START ART BASED ON CD4 COUNT.