AUGUST ASSESSMENT

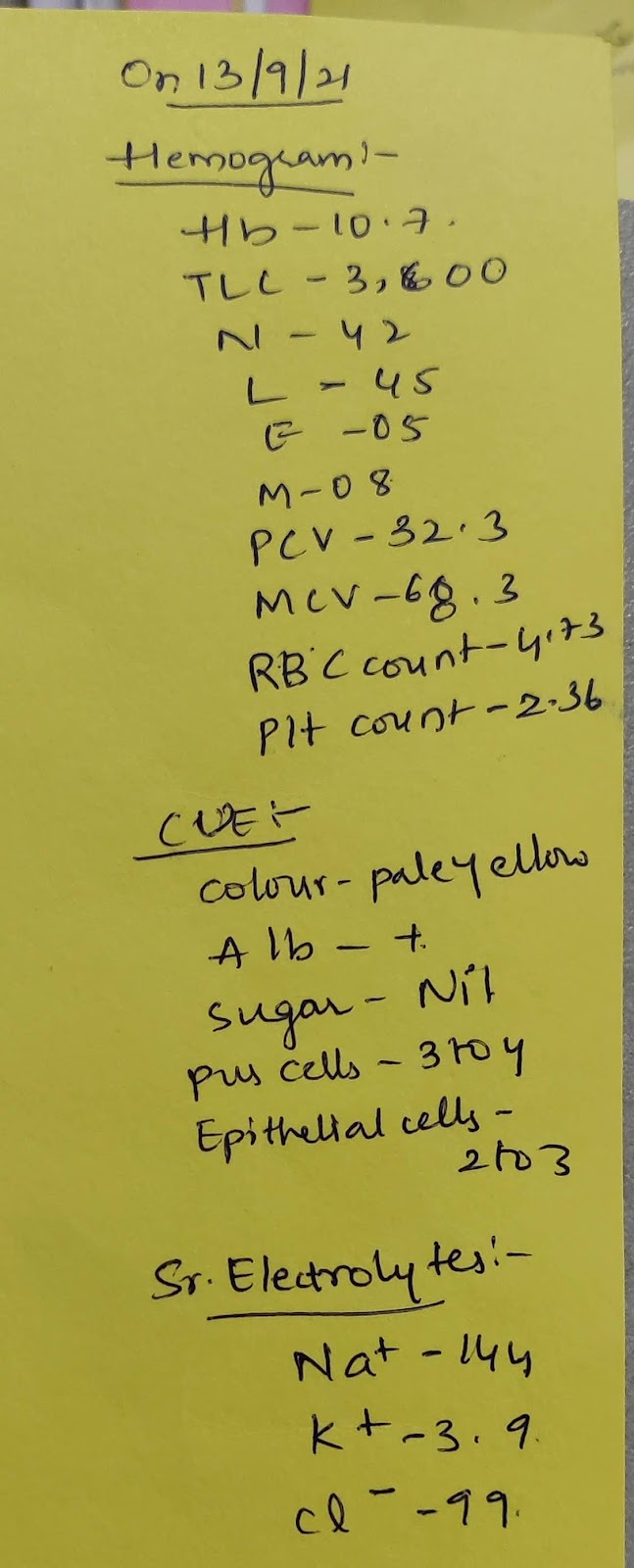
LONG CASE Q1) (Testing peer review competency in the active reader of this assignment) : Please go through the long and short cases in the first link shared above and provide your critical appraisal of the captured data in terms of completeness, correctness and ability to provide useful leads to analyze the diagnostic and therapeutic uncertainties around the cases shared. Please provide your peer review assessment on not only the the student's written case report but also the reading of the cases followed by the question answer session linked above in the video and share your thoughts around each answer by the student along with your qualitative insights into what was good or bad about the answer. OVERVIEW A 44 year old man presented with a 3-day history of bilaterally symmetrical rapidly progressive generalized edema. he noticed he started feeling facial puffiness with pedal edema, the next morning he noticed facial puffiness. At the same time, he also noticed that he developed bi...